It’s believed that up to 17 percent of the population has mast cell activation syndrome, or MCAS for short.
Yet it’s one of the most unrecognized and under-addressed chronic conditions, and until 2016 wasn’t officially recognized as a diagnosis.
Even with its lack of notoriety, MCAS is a trending phenomenon. There are millions of TikTok and other social media videos on the topic, so awareness is increasing.
What is mast cell activation syndrome, and what can be done about it?
What Are Mast Cells?
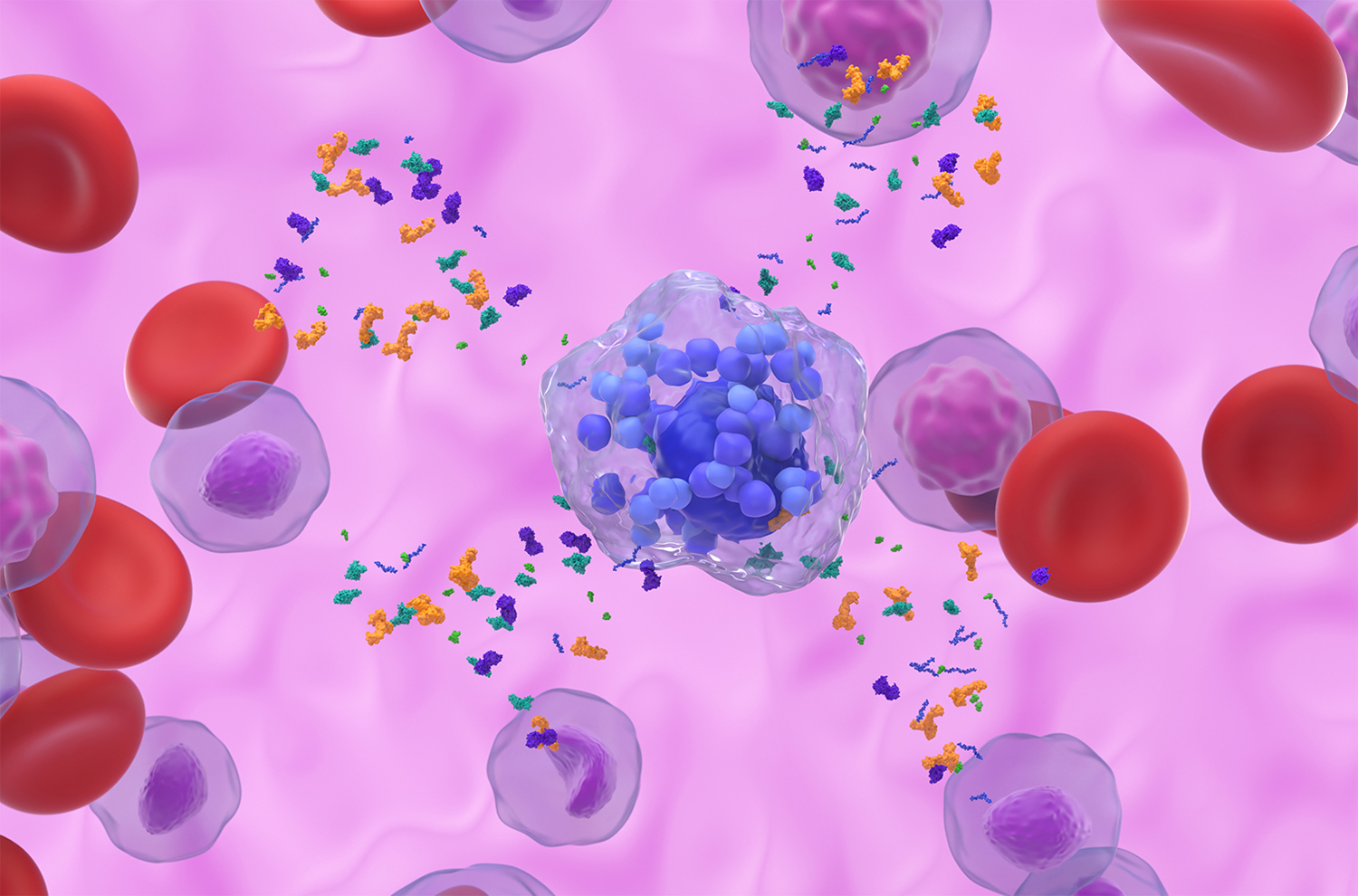
A team of infection-fighting white blood cells, mast cells are an important part of the immune system. Mast cells are in almost every tissue of the body, including:
- the skin
- the GI tract
- blood vessels
- nerves
- bones
- the brain
- the lungs
- the eyes
- the ears
What Do Mast Cells Do?
Mast cells are necessary for our survival, protecting us from invading pathogens and harmful substances, and helping with wound repair.
What is Mast Cell Activation Syndrome?
When triggered into an overreaction phase, mast cells mistakenly alert the immune system that something’s off.
This false alarm causes the body to release high amounts of inflammatory mediators like histamine, as well as other chemicals that trigger the immune system into action. These chemical mediators activate even more mast cells to respond.
Over time, the mast cells start seeing almost everything as a threat.
What Causes MCAS?
Experts aren’t sure why some individuals’ mast cells overreact. While mast cell activation syndrome is not an autoimmune issue, if the immune system becomes overwhelmed and something comes along that pushes it over the edge, mast cell activation syndrome can occur in some people.
Traumatic medical events like surgery, injury, or illness; exposure to insect or reptile venom; medications; stress; and infections can all trigger MCAS.
Certain smells can be a problem too. A walk down the grocery aisle of laundry detergents and cleaning formulas with their synthetic fragrances can trigger a mast cell attack.
Types of MCAS
There are different types of mast cell activation.
-
Genetic
One is associated with genetic conditions that are linked to mastocytosis (a type of rare mast cell disease where the body produces too many mast cells).
-
Allergic
Another type of MCAS is triggered by certain allergies.
-
Idiopathic
A third variety is known as idiopathic mast cell activation syndrome. It has no determinable cause, as it’s not related to other diseases or clear issues.
Those experiencing this type of MCAS have new triggers that come up and cause reactions.
How Do I Know If I Have MCAS?
Lab tests tend to be inconclusive, since the blood only shows spikes above the baseline for a few hours after an attack. Because of this, levels are tested not only when someone’s having an episode but also when they’re feeling fine.
Diagnosis typically requires that symptoms occur in at least two of the following areas: the skin, the lungs, the GI tract, and the cardiovascular system.
Some practitioners feel that symptoms must be so severe that they resemble anaphylaxis. However, the debate continues on how extreme or consistent symptoms must be in order to be considered part of MCAS.
Speaking of symptoms: one person’s presentation can be completely different from another’s. In fact, medical practitioners often misdiagnose mast cell activation syndrome for other conditions due to the multitude of conditions it causes.
Some professionals feel that MCAS is diagnosed too often.
Symptoms of MCAS
Mast cell activation syndrome symptoms vary from the mild to the rare and life-threatening, including anaphylaxis when swelling, hives, shortness of breath, and vomiting.
In less severe forms of MCAS, symptoms are varied and may include:
- abdominal pain
- brain fog
- chronic gut issues
- constipation
- diarrhea
- excessive drooling
- fatigue
- flushing
- food sensitivities and allergies
- heart palpitations
- increased heart rate
- insomnia
- itching
- joint pain
- lightheadedness
- low blood pressure
- muscle weakness
- numbness
- sensitivity to light or sound
- shortness of breath
- sinus congestion
- skin conditions:
- rashes
- rosacea
- psoriasis
- eczema
- swelling
- tingling
- tinnitus
It’s important to note that those with MCAS may notice symptoms randomly appearing and disappearing, and they may have difficulty determining the triggers.
What makes mast cell activation syndrome even more confusing is that symptoms can increase, change, and even worsen over time.
Many of the above symptoms can also be linked to other disorders such as postural orthostatic tachycardia syndrome (POTS), IBS, and Ehlers-Danlos Syndrome (EDS).
MCAS Treatments
There’s currently no cure for MCAS, nor are there any fast fixes. But research is expanding, and those who suffer from its debilitating cluster of symptoms can often find relief.
Mast cell activation syndrome is frequently managed with medications and other treatments.
-
Identify and Avoid Triggers
Trigger avoidance is key to preventing mast cells from overreacting.
Track your symptoms with a journal. List the foods you ate and any irritants you were exposed to.
This can help you determine possible triggers like:
- pet dander
- plant pollen
- bee venom
- certain foods
- toxic mold
- chemical exposure
- heavy metal exposure
Nervous system dysregulation, temperature changes, exercise, lack of sleep, and stress can also be triggering.
-
Stress Relief
Practice stress-relieving tactics such as meditation, mindfulness techniques, resting, spending time with friends, and participating in a hobby. Supporting the nervous system can also be profoundly helpful.
-
Try Over-the-Counter Meds
Aspirin can help with flushing. Over-the-counter antihistamine formulas can help rid the body of inflammation.
-
Seek Corticosteroids
Corticosteroids may be prescribed to reduce inflammation and open airways.
-
Seek Mast Cell Stabilizers
Mast cell stabilizers can help regulate overreacting mast cells. When anaphylaxis is a concern, an EpiPen® will be prescribed.
Keep in mind that if mast cell medications offer symptom relief, it’s a probable sign that you have mast cell activation syndrome.
-
Consider Supplements
-
Quercetin for GABA Help
For supplemental help, consider quercetin. GABA has been shown to inhibit mast cell activation, which can reduce the release of histamine and other pro-inflammatory substances.
-
CoQ10 for Energy
Consider CoQ10 for mitochondrial and energy support.
-
The COVID Link
Those experiencing Long COVID have an increase in MCAS and its symptoms.
-
Comorbidity
A published study found an increase in MCAS triggered by SARS-CoV-2. Researchers theorized that increased mast cell activation due to COVID-19 infection may contribute to Long COVID.
-
Overlapping Symptoms
There’s a definite overlap in symptoms experienced in MCAS and Long COVID. In fact, they’re virtually identical, and can include:
- anxiety
- depression
- migraines
- brain fog
- fatigue
- coughing
- sore throat
- bloating
- diarrhea
- constipation
- food intolerances
- chest pain
- heart palpitations
Precautions
-
Seek Medical Advice
See a doctor if you’re experience new or worsening symptoms to rule out serious issues.
-
React to Emergencies
Severe reactions from MCAS are rare, but if a serious allergy occurs (trouble breathing or swallowing; fast heart rate; swelling of the lips, face, tongue, or throat) call 911 or go to the emergency room.